Treatment of Hypertension or High Blood Pressure
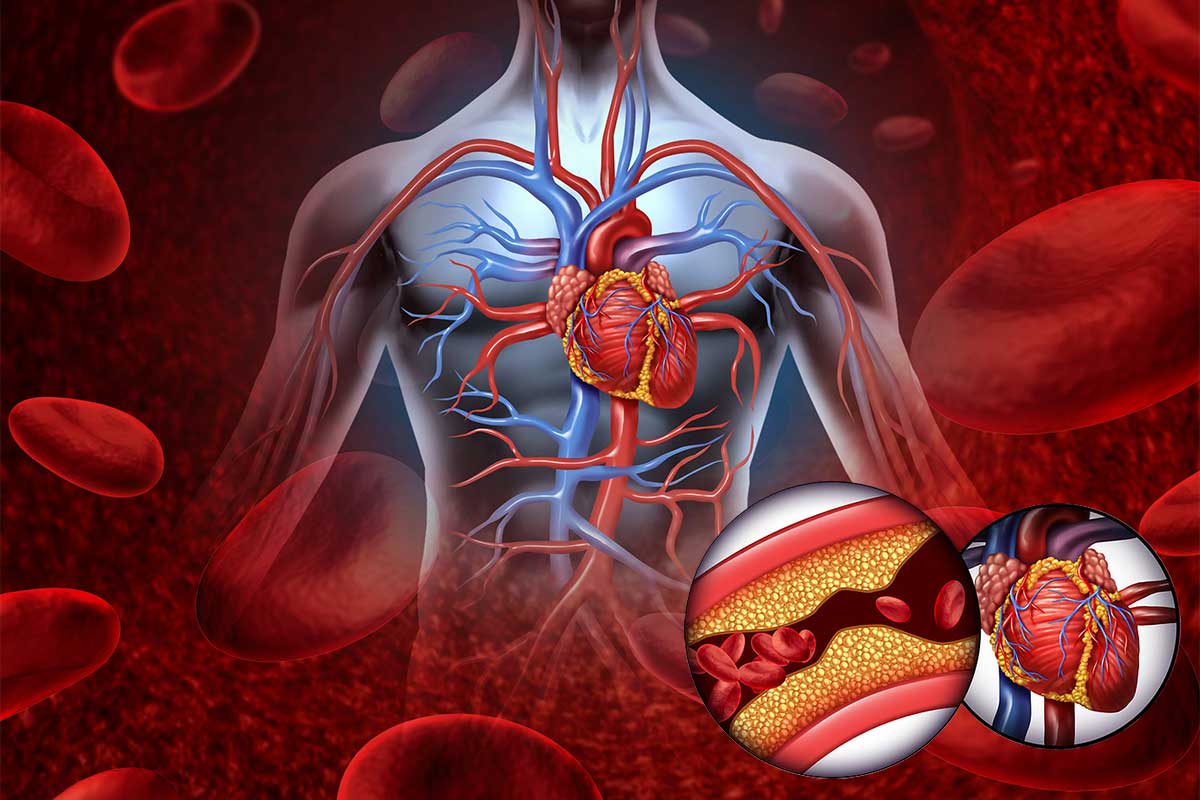
Having hypertension puts patients at higher risk of diseases such as heart attacks and strokes. Other consequences from hypertension include chronic kidney disease, damage to the eyes, headaches, and irregular heart rhythms.
The Covid-19 pandemic has been the centerpiece of change for everyone throughout the world. It permeated the mindspace for all walks of life and put pressure on healthcare systems in more ways than one. During these challenging times, Family Medicine physicians and other primary care providers did their best to keep patients out of the hospital while keeping themselves safe amidst the Covid pandemic. Managing diseases such as hypertension, hyperlipidemia, coronary artery disease, heart failure, type 2 diabetes mellitus, chronic kidney disease, and COPD via telehealth had its challenges requiring teamwork and sacrifices from all parties involved. As a board-certified Family Medicine physician, I’d like to share some of my experiences managing hypertension in the setting of a global pandemic.
Let’s begin with discussion with how hypertension is defined. This may be surprising but not all organizations or societies share the same definition of hypertension. From a primary care standpoint, the Joint National Commission and the American College of Cardiology/American Heart Association are the two predominant organizations used for managing hypertension. The Joint National Commission (or JNC) 8th report says a patient should start treatment for hypertension for blood pressure reading of systolic blood pressure (top number) of greater than or equal to 140 and/or diastolic blood pressure (bottom number) greater than or equal to 90. For patients 60 years old and older, treatment goal should be less than 150 systolic over 90 diastolic. To further convolute this, if a patient has diabetes or chronic kidney disease, treatment goals should be to less than 140 systolic over 90 diastolic regardless of age. The American College of Cardiology/American Heart association defines hypertension as two separate readings- clinical and at home- of systolic reading 130 or more, and diastolic reading of 80 or more.
So, who do we follow? To simplify things, less than 140/90 is acceptable, and less than 130/80 is better. You may be asking “why should we care about hypertension in the first place”? As a primary care physician, it’s my job to help improve the quality of life of my patients by managing their health. Having hypertension puts patients at higher risk of diseases such as heart attacks and strokes. Other consequences from hypertension include chronic kidney disease, damage to the eyes, headaches, and irregular heart rhythms. Fortunately for us, we can do something about it!
First, we screen patients 18 years of age and older. From there, we start discussing risk factors or other disease states that can have a negative impact and determine an overall risk So after finding our patients, what’s next?
Signup today and find a doctor near you
Probably the most important aspect of treatment (and the one that requires the most discipline) is lifestyle modification. Diet and exercise are the two primary areas we focus on. Restricting salt intake can have a huge impact on controlling blood pressure. Limiting salt intake to 1000 mg per day is ideal but up to 1500 mg per day is considered acceptable. Did you know processed foods contain more salt than freshly prepared foods? Preparing and cooking your own food is a good approach and can drop your BP 5-6 mm Hg. Limiting the number of times you eat fast food will also help. Shop the “outside” isles of the grocery store looking for fresh foods and reading the labels are tips to help reduce salt intake.
Weight loss is another lifestyle modification, which can lead to 0.5 mmHg to 2 mmHg for every 2 lbs lost. This is typically done with an extra 30 minutes of moderate intensity exercise per day (light walking) or 150 min per week, which is not included in daily activity such as work. Exercise can drop your BP 3-6 mmHg independent of weight loss. Other lifestyle modifications include limiting alcohol intake, stop smoking, and the DASH diet.
In addition to lifestyle modification, medications are the next best step! Without getting into too much detail, three main groups of medications are used. The first are ACE inhibitors/ARBs such as Lisinopril or Losartan. This class can also help with protecting the kidneys and in some cases, protecting the heart. A second class of medications are the calcium channel blockers such as Amlodipine or Nifedipine. Finally, a third class commonly used are thiazide diuretics (water pills) such as Hydrochlorothiazide and Chlorthalidone. Any of these would be a good choice alone or sometimes in combination. Speak to your doctor if you have questions!
As you start to see your Family Physician again during this pandemic, remember to ask him or her about your blood pressure. Specifically, ask about how to properly monitor it at home and things you can do to help keep it controlled. As we navigate through this pandemic together, it’s important for us to continue to be resourceful in maintaining good health by seeing your primary care provider, doing what you can at home with lifestyle changes, and following the plan of action you put together with your doctor.





